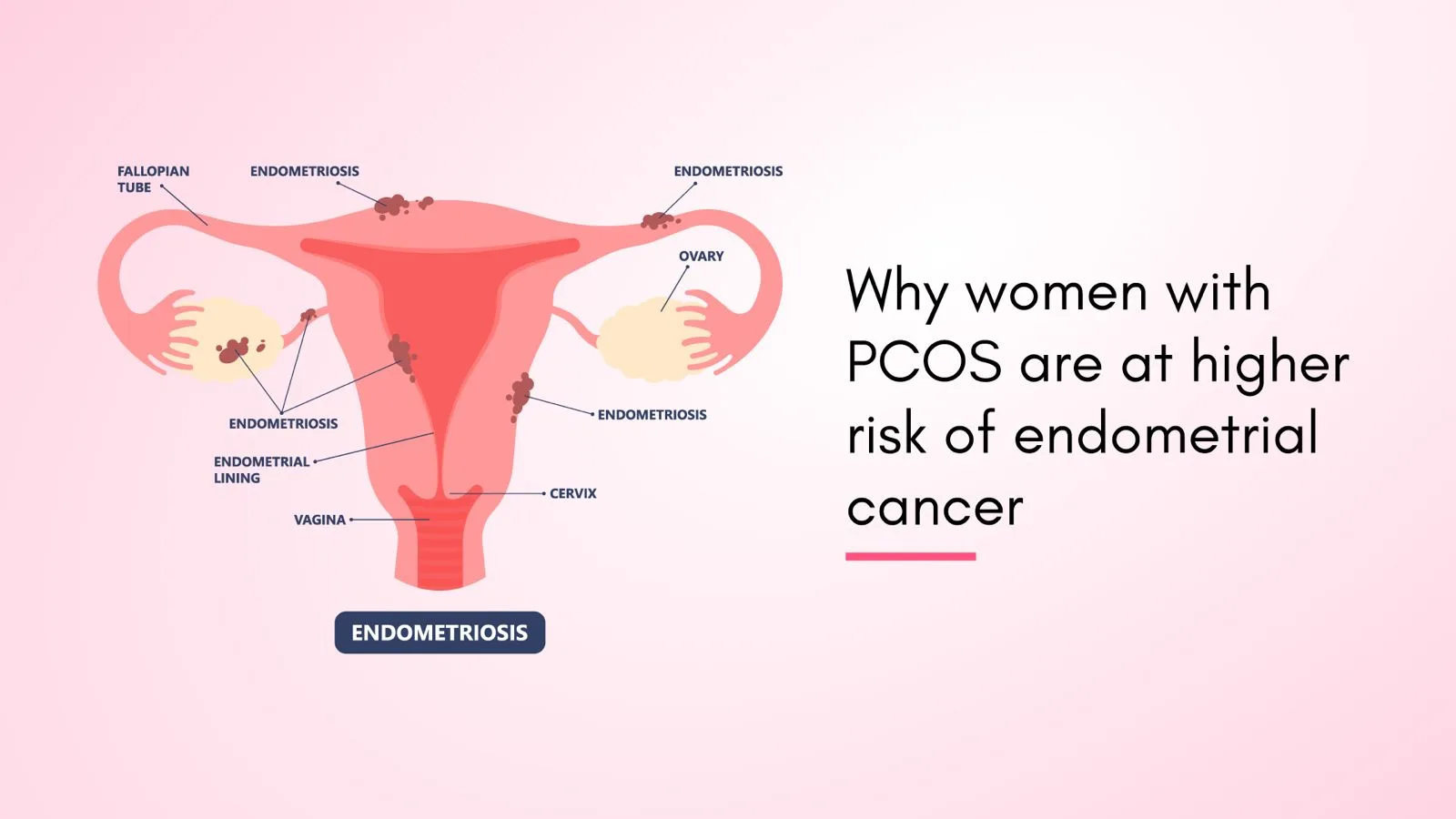
What is Endometrial Cancer?
Cancer that originates in the uterine lining, or endometrium (womb), is known as endometrial cancer. Endometrial cancer is the most recurring gynecologic malignancy, accounting for 7% of all women’s cancers. Of all uterine cancers, endometrial cancer is the second most frequent. The exact cause of endometrial cancer is uncertain. One possible explanation is a rise in the hormone estrogen. This causes the uterine lining to thicken, which may result in cancer and aberrant endometrial development. Between the ages of 60 and 70, endometrial cancer typically manifests itself. A few instances might arise before the age of 40.
Suggested Read: Fertility Preservation Options For Cancer Patients
PCOS and its Impact on Hormones
For women of reproductive age, PCOS is a highly prevalent hormonal issue. Sometimes, a woman produces insufficient amounts of the hormones required for ovulation. In addition to having high testosterone levels, when ovulation is unsuccessful, the ovaries may produce several little sacs filled with fluid (cysts). These cysts produce androgen, and women with PCOS often have elevated levels of androgen. This can create more problems with a woman’s menstrual cycle, and furthermore, it can induce many symptoms of PCOS. Infertility, weight gain, acne, irregular or skipped menstrual cycles, and increased hair growth are all possible side effects of PCOS.
Suggested Read: Surprising Causes of Low Testosterone Levels
The Connection Between PCOS and Endometrial Cancer
Polycystic ovarian syndrome (PCOS) is a prevalent endocrine condition that affects 4-21% of women of reproductive age. An increased risk of endometrial cancer has been found in females with PCOS, while the underlying mechanism remains unknown. Endocrinologic and metabolic abnormalities reported in PCOS may have complicated consequences on the endometrium, such as an increase in the expression of androgen and steroid receptors, contributing to endometrial dysfunction. The long-term problems of PCOS include obesity, unopposed estrogen in anovulatory females, insulin resistance, nulliparity, and diabetes, all of which are significant risk factors for endometrial cancer.
Suggested Read: PCOS treatment in Hyderabad
Endometrial Cancer Symptoms
Abnormal Vaginal Bleeding
The most prevalent indication of endometrial cancer is irregular vaginal bleeding. It usually happens early in the disease process, which is why most patients are identified with curable stage I endometrial cancer.
Pelvic Pain
Lower abdominal discomfort or pelvic cramps. Some people have pain during urinating or difficulty emptying their bladder. As the disease advances, you may feel heaviness in your pelvis.
Abnormal Vaginal Discharge
Endometrial cancer in some women produces a thin, watery, or yellowish discharge.
Pain During Intercourse
Endometrial cancer can induce pelvic discomfort, though this is less prevalent during sexual intercourse.
Unexplained Weight Loss
Another indicator of uterine cancer is unintentional weight loss. Unexplained weight loss may not be significant, but it can also indicate other sorts of cancer, so a person should always consult a doctor if they lose weight without trying.
Enlarged Abdomen or Bloating
Symptoms of advanced endometrial cancer include stomach or pelvic discomfort, bloating, feeling full immediately after eating, and changes in bowel or bladder habits.
Fatigue
Cancer-related fatigue (CRF) is the most prevalent complaint among patients with gynecological malignancies. CRF is sometimes neglected, although it can significantly reduce patients’ quality of life.
Frequent Urination
In the late stages of endometrial cancer, a person may have bladder and bowel problems such as frequent urination or constipation.
Suggested Read: Earlier Detection of PCOS for Fertility Preservation
Risk Factors of Endometrial Cancer
Hormonal Imbalances
The ovaries produce two primary hormones: estrogen and progesterone. Changes in the balance of these hormones affect the endometrium, and an increase in estrogen levels can elevate endometrial cancer risk.
Obesity and Overweight
Obesity is the biggest risk factor for endometrial cancer, and it increases the risk of the illness by 60% for every 5kg/m2 rise in BMI.
Age
The probability of having uterine cancer rises with age. Women diagnosed with endometrial cancer are typically 60 years old. In women younger than 45, it is rare.
Family History and Genetics
There is an increased chance of endometrial cancer among females who have at least one first-degree family member (mother, sister, or daughter) who has the disease.
Menstrual Irregularities
The uterine lining may thicken as a result of certain disorders that produce irregular and less frequent menstruation (endometrial hyperplasia). If left untreated, endometrial hyperplasia may develop into endometrial carcinoma.
Lifestyle Factors
Globally, obesity and physical inactivity are two major modifiable lifestyle variables that significantly increase the risk of endometrial cancer.
Suggested Read: PCOS Fertility Issues and Solutions
Why PCOS Increases the Risk of Endometrial Cancer?
Elevated Estrogen Levels
The endometrium, or uterus lining, can be significantly impacted by these hormonal abnormalities, especially elevated levels of estrogen, which can increase the risk of endometrial cancer.
Irregular Menstrual Cycles
PCOS causes anovulation and an imbalance in reproductive hormones, leading to irregular menstrual cycles. This irregularity or absence of a menstrual cycle leads to a condition called endometrial hyperplasia. If endometrial hyperplasia is left untreated, it can increase the risk of endometrial cancer.
Insulin Resistance and Obesity
One of the risk factors for endometrial cancer is insulin resistance. Numerous physiological processes that promote carcinogenesis can be triggered by hyperinsulinemia (high insulin levels in the blood). According to reports, between 65% and 70% of women with PCOS have insulin resistance. A prevalent characteristic of PCOS is obesity, and compared to thinner women with the illness, obese women with PCOS had more aberrant endocrine and metabolic profiles.
Metabolic Syndrome and Inflammation
Among the numerous related risk factors, metabolic syndrome (MetS) is a significant one that may be avoided. It consists of central obesity, hyperglycemia, arterial hypertension, and atherogenic dyslipidemia, which frequently coexist.
Lack of progesterone
Polycystic ovarian syndrome (PCOS) is characterized by abnormal steroid hormone synthesis and activity. Chronic estrogen exposure or a lack of progesterone owing to ovarian malfunction can cause endometrial hyperplasia and cancer.
Genetic and Environmental Factors
The cause of this illness is a combination of hereditary and environmental factors. An unhealthy lifestyle, nutrition, or any viral mediators all raise the chance of PCOS.
Endocrine Disruptions
Endometrial, ovarian, and breast cancers are all associated with chronic hormone stimulation in women. Chronic estrogen stimulation in women with PCOS frequently leads to endometrial hyperplasia or malignancy.
Psychological Stress and Lifestyle Factors
The relationship between PCOS and mental health is complicated, with people frequently dealing with increased risks of anxiety and depression. PCOS-related hormonal abnormalities can cause mood swings, increasing the likelihood of depressive symptoms and anxiety disorders.
How to Reduce the Risk of Endometrial Cancer for Women with PCOS?
Frequently, obese or overweight women have PCOS. Being obese raises estrogen levels, which is a known risk factor for endometrial cancer. Even with PCOS, women can reduce their risk of endometrial cancer and shed extra pounds by exercising regularly and maintaining a nutritious diet.
Conclusion
Usually, endometrial cancer is discovered early on. The survival rate is high in the first five years after diagnosis, and after five years, roughly 25% of women still live if the disease has progressed to distant organs. By engaging in physical exercise and maintaining a healthy lifestyle, you can avoid hormonal imbalances and other metabolic illnesses linked to PCOS and endometrial cancer.