Infertility can be a challenging and emotional phase that affects millions of couples worldwide. For men with azoospermia, a condition where no sperm is present in the ejaculate, the dream of becoming a father can feel out of reach. But there is hope. A special procedure called Micro-TESE (Microscopic Testicular Sperm Extraction) has changed the game, offering the chance for biological parenthood.
In this blog, we will discuss Micro-TESE. We’ll explore how it works, when it’s needed, the risks involved, and the detailed steps of the procedure. By the end, you’ll have a clear understanding of why this innovative approach is giving new hope to many individuals and couples facing male infertility and bringing them closer to their dream of having a child.
Also Read: Fertility and Nutrition: Foods and Supplements That May Boost Male Fertility
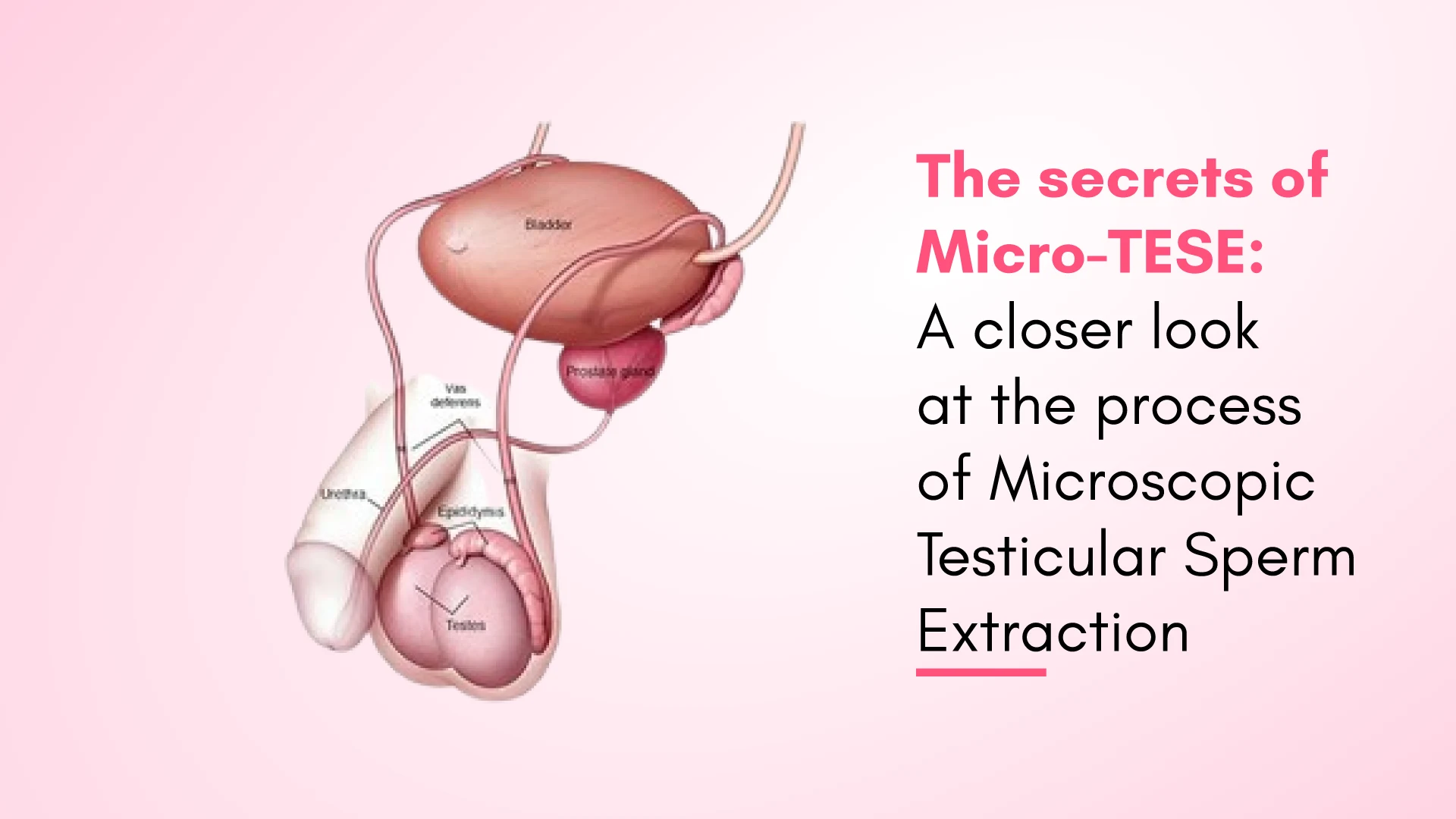
What is a Micro-TESE?
Micro-TESE, or Microscopic Testicular Sperm Extraction, is a specialised surgical procedure used to retrieve sperm from the testes of men who have been diagnosed with azoospermia, a condition characterised by the complete absence of sperm in the ejaculate. Highly skilled urologists or reproductive endocrinologists perform this procedure, who utilise a microscope to meticulously search for and extract viable sperm directly from the testicular tissue.
The primary goal of a Micro-TESE is to identify and collect the small pockets of sperm that may be present within the testes, even in cases where no sperm are visible in the semen. This collected sperm can then be used for assisted reproductive techniques, intracytoplasmic sperm injection (ICSI), to help couples struggling with infertility realise their dream of starting a family.
Types of Micro-TESE
There are two main types of Micro-TESE procedures:
- Conventional Micro-TESE: In this approach, the surgeon makes a small incision in the scrotum and examines the testicular tissue under a high-powered microscope to identify and extract the sperm-containing tubules.
- Micro-TESE with Testicular Mapping:
This technique involves a more comprehensive approach, where the surgeon first maps out the testicular tissue using a grid system to identify the areas with the highest sperm concentration. The surgeon then focuses the microscopic search on these targeted regions, increasing the chances of successful sperm retrieval.
Also Read: The Impact Of Age On Fertility: When To Consider Seeking Assistance
What are the Indications of a Micro-TESE?
Micro-TESE is typically recommended for men who have been diagnosed with medical conditions including but not limited to:
- Azoospermia: A state of zero sperm or complete absence of sperm in the ejaculate. It can be due to underlying conditions, such as congenital obstructions, genetic disorders, or previous testicular injury or surgery.
- Severe Oligospermia: Extremely low count of sperm, where the number of sperm in the ejaculate is significantly lowered, often to less than 1 million per millilitre.
- Failed Previous Sperm Retrieval Attempts: Men who have undergone previous sperm retrieval procedures, such as conventional testicular biopsy or TESE, without success may be candidates for a micro-TESE.
- Idiopathic Infertility: In cases where the cause of male infertility is unknown, doctors may recommend micro-TESE to retrieve sperm for assisted reproductive techniques.
- Cryptorchidism: Men with undescended testicles (cryptorchidism) in childhood may have compromised sperm production and may be candidates for a micro-TESE.
Related Read: 10 Surprising Causes of Low Testosterone Levels
Risks of Micro-TESE
While Micro-TESE is generally considered safe and effective. There may be some risks and complications that patients should be aware of, including:
- Bleeding: There is a small risk of bleeding during or after the procedure, which may require additional treatment or hospitalisation.
- Infection: As with any other surgical procedure, there is a chance of infection at the incision site, which may require antibiotic therapy.
- Testicular Damage: In rare cases, the procedure may damage the testicular tissue, decreasing testosterone production or other hormonal imbalances.
- Anaesthesia Complications: Using general or local anaesthesia during the procedure carries the typical risks associated with these types of anaesthesia, such as allergic reactions or nausea.
Patients must discuss the probability of these risks with their doctor and follow all pre-and post-operative instructions to the core to minimise the likelihood of complications.
Related Read: Why Is Male Infertility on the Rise in India?
How is the Micro-TESE Procedure Done?
Before the Procedure
Before the Micro-TESE procedure, the patient will undergo a comprehensive medical evaluation, which may include:
- Detailed Medical History: The doctor will review the patient’s medical history, including previous fertility treatments, surgeries, or underlying medical conditions.
- Physical Examination: The fertility specialist will conduct a thorough physical evaluation, focusing on the genital area and checking for abnormalities or signs of obstruction.
- Hormonal Evaluation: Blood tests may help assess the patient’s levels of crucial reproductive hormones, such as testosterone, follicle-stimulating hormone (FSH), and luteinising hormone (LH).
- Semen Analysis: The patient will provide a semen sample, which will be analysed to confirm the diagnosis of azoospermia or severe oligospermia.
- The doctor may also recommend the patient discontinue certain medications or supplements in the weeks before the procedure.
During the Procedure
The Micro-TESE procedure is typically performed under general or local anaesthesia with sedation. The steps of this procedure are as follows:
- Incision: The surgeon makes a small incision in the scrotum, exposing the testes.
- Microscopic Examination: The surgeon will carefully examine the testicular tissue using a high-powered microscope, searching for tiny pockets of sperm-containing tubules.
- Sperm Retrieval: Once the sperm-containing areas are identified, the surgeon gently extracts small tissue samples, which are examined under the microscope to confirm the presence of viable sperm.
- Closure: After the sperm retrieval is complete, the surgeon closes the incision area with the help of sutures or other closure methods.
After the Procedure
Following the Micro-TESE procedure, the patient will be monitored briefly to ensure no immediate complications, such as bleeding or infection. The patient may experience discomfort or swelling in the scrotum, which can be effectively managed with pain medication and ice packs.
The retrieved sperm samples will be carefully processed and cryopreserved (frozen) for future use in assisted reproductive treatments, such as IVF or ICSI.
The medical team will advise the patient to avoid strenuous activity for a week or two and to follow any specific post-operative instructions provided by the gynaecological surgeon.
Why Choose Ferty9 for Micro-TESE?
At Ferty9, we understand the deeply personal and emotional journey of infertility. That’s why we have assembled a team of highly trained, experienced, skilled, and compassionate professionals dedicated to providing world-class care and support throughout the Micro-TESE process.
Some of the key reasons why Ferty9 is the preferred choice for Micro-TESE include:
- Expertise and Experience: Our board-certified reproductive surgeons have extensive experience performing Micro-TESE procedures, ensuring the best possible outcomes for our patients.
- Advanced Technology: We utilise the latest advancements in microscopic technology and laboratory techniques to maximise the chances of successful sperm retrieval.
- Personalised Approach: We take the time to understand each patient’s unique circumstances and tailor your treatment plan accordingly, ensuring a truly personalised experience.
- Compassionate Care: We recognise the emotional toll that infertility can take. Our team works closely with you and creates a supportive and empathetic environment.
- Comprehensive Services: In addition to Micro-TESE, we offer a full range of fertility treatments and support services to help our patients achieve their family-building goals.
Also Read: IVF cost – Myths and facts, inclusions, Ferty9’s promise of affordability
Conclusion
Micro-TESE is a highly specialised and delicate procedure that offers hope to many men struggling with azoospermia or severe oligospermia. By utilising the power of microscopic technology, skilled surgeons can meticulously search for and extract the elusive sperm that may be present within the testes, providing couples with a path forward in their journey to start a family.
While the procedure does carry some risks, the potential benefits of successful sperm retrieval and the ability to pursue assisted reproductive treatments can make Micro-TESE a life-changing option for those facing infertility challenges. Patients considering this procedure should work closely with their doctors to understand the process, weigh the risks and benefits, and determine if Micro-TESE is the right choice for their unique situation.